Lung Function Testing
Flow Volume Loops (Spirometry)
Spirometry is a common pulmonary function test that measures the amount of air a patient can inhale and exhale, as well as the speed at which they can do so. Specifically, spirometry measures two key parameters:
Forced Expiratory Volume in 1 second (FEV1) - the amount of air that can be forcefully exhaled in one second.
Forced Vital Capacity (FVC) - the total amount of air that can be exhaled forcefully after taking a deep breath.
Spirometry can provide important information about lung function, particularly in the diagnosis and management of obstructive lung diseases such as asthma and chronic obstructive pulmonary disease (COPD). However, it does not provide information about gas transfer across the lung tissue or lung volumes, which can be important in the diagnosis and management of other lung conditions.
Adding DLCO and lung volume testing to spirometry can provide a more complete picture of a patient's lung function. DLCO, or diffusing capacity of the lung for carbon monoxide, measures how well the lungs are able to transfer gases from the air into the bloodstream. This test can be particularly useful in the diagnosis and management of interstitial lung disease, pulmonary hypertension, and emphysema.
Lung volume testing, such as body plethysmography, measures the amount of air in the lungs at different stages of breathing. This type of testing can help in the diagnosis and management of restrictive lung diseases, neuromuscular disorders, and other conditions that affect lung volumes.
By adding DLCO and lung volume testing to spirometry, a GP can obtain a more complete picture of a patient's lung function. This can help in the diagnosis and management of a wide range of lung conditions, particularly those that may not be fully captured by spirometry alone. Additionally, having a more complete understanding of a patient's lung function can help guide treatment decisions and monitor the response to treatment over time.
Lung Function Testing
BLUK BILLING FOR ROUTINE LUNG FUNTION TESTING
Lung function testing, also known as pulmonary function testing, is a medical exam that measures how well your lungs are working. During the test, you will breathe into a machine that will measure the amount of air you inhale and exhale, as well as how quickly you do it.
This test is beneficial because it can help your doctor diagnose lung conditions such as asthma, chronic obstructive pulmonary disease (COPD), and pulmonary fibrosis. Lung function testing can also help your doctor monitor the progression of your lung disease and evaluate the effectiveness of your treatment plan.
If your doctor has recommended lung function testing for you, it is important to follow their instructions and attend the appointment. The test is non-invasive and usually takes less than an hour to complete. By understanding how well your lungs are functioning, you can take steps to manage your condition and improve your overall health
Asthma first aid
Please follow the link below for advice on how to manage an asthma attack https://www.nationalasthma.org.au/asthma-first-aid
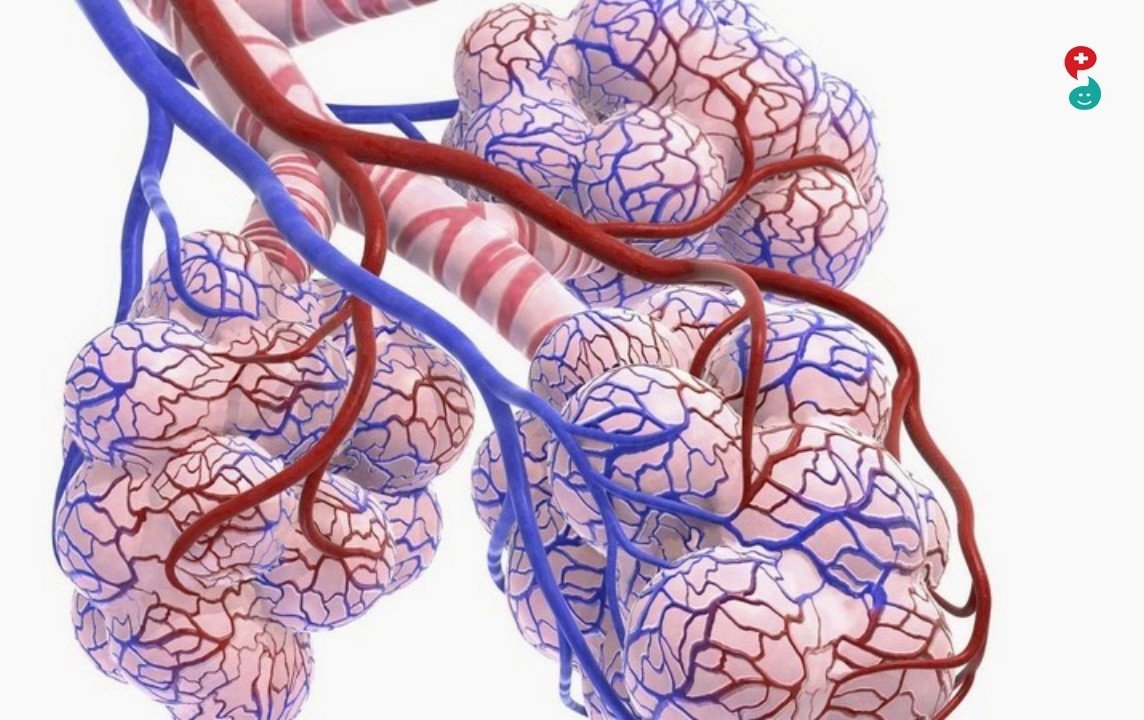
Diffusion Capacity
DLCO stands for "diffusing capacity of the lung for carbon monoxide". It is a lung function test that measures the ability of the lungs to transfer gases from the air into the bloodstream. Specifically, it measures how well the lungs are able to transfer carbon monoxide (CO) from a gas mixture into the bloodstream.
The DLCO test provides additional information about lung function that cannot be obtained from spirometry alone. While spirometry measures the amount of air that can be forcefully exhaled in one second (FEV1) and the total amount of air exhaled (FVC), it does not provide information about gas transfer across the lung tissue.
DLCO can help in the diagnosis of several lung conditions, including chronic obstructive pulmonary disease (COPD), interstitial lung disease, pulmonary hypertension, and emphysema. It can also help in monitoring the progression of these diseases over time.
DLCO is a safe and non-invasive test that is usually performed in a pulmonary function laboratory. The patient breathes into a machine that measures the concentration of carbon monoxide in the air they inhale and exhale. The results are reported as a percentage of the expected value based on age, gender, and height.
In summary, DLCO is a valuable test that provides important information about lung function beyond what can be obtained from spirometry alone. It can help in the diagnosis and management of several lung conditions, and is a safe and non-invasive test that can be easily performed in a pulmonary function laboratory.
Examination of the Carbon Monoxide Diffusing Capacity (DLCO) in Relation to Its KCO and VA Components https://www.atsjournals.org/doi/pdf/10.1164/rccm.201112-2160CI
What can we learn from pulmonary function testing in heart failure?European Journal of Heart Failure (2017) 19, 1222–1229 doi:10.1002/ejhf.946
Lung Volumes
Lung volumes are a set of measurements that describe the amount of air in the lungs at different stages of breathing. These measurements include:
Total Lung Capacity (TLC) - the total amount of air the lungs can hold when they are completely filled.
Residual Volume (RV) - the amount of air left in the lungs after a complete exhalation.
Inspiratory Reserve Volume (IRV) - the additional air that can be breathed in after a normal inhalation.
Expiratory Reserve Volume (ERV) - the additional air that can be breathed out after a normal exhalation.
Vital Capacity (VC) - the maximum amount of air that can be exhaled after a deep inhalation.
Functional Residual Capacity (FRC) - the amount of air left in the lungs after a normal exhalation.
Body plethysmography is a technique used to measure lung volumes. During this test, the patient sits inside a sealed, transparent chamber called a plethysmograph. They are then asked to breathe through a mouthpiece and nose clip while measurements are taken. The plethysmograph measures the changes in air pressure that occur as the patient breathes, allowing the calculation of lung volumes.
The benefits of requesting lung volume testing in addition to spirometry include:
A more complete assessment of lung function: While spirometry is a valuable test that provides information about airflow obstruction, it does not measure lung volumes. By requesting lung volume testing, a GP can obtain a more complete picture of the patient's lung function.
Improved diagnosis of lung conditions: Lung volume testing can help in the diagnosis of several lung conditions, such as chronic obstructive pulmonary disease (COPD), restrictive lung diseases, and neuromuscular disorders. It can also help to differentiate between obstructive and restrictive lung diseases.
Better management of lung conditions: Measuring lung volumes can help in the management of lung conditions by providing information about the severity and progression of the disease. It can also help to guide treatment decisions and monitor the response to treatment.
In summary, lung volume testing using body plethysmography is a valuable tool that can provide important information about lung function beyond what can be obtained from spirometry alone. It can help in the diagnosis and management of several lung conditions, and is a safe and non-invasive test that can be easily performed in a pulmonary function laboratory.
Standardisation of the measurement of lung volumes.
The Benefits of Using a Spacer with Your Salbutamol Inhaler
A spacer is a simple device that can significantly improve the effectiveness of your salbutamol inhaler. It acts as a holding chamber for the medication, giving you more time to inhale it properly. Here are some key advantages:
Better Medication Delivery: Using a spacer ensures that more of the salbutamol reaches your lungs rather than getting stuck in your mouth or throat. This can lead to better control of asthma symptoms.
Easier to Use: With a spacer, you don’t need to perfectly time the pressing of the inhaler with your breathing. It allows for a more gradual and controlled inhalation, making it especially helpful for children or those who struggle with inhaler technique.
Reduced Side Effects: By preventing the medication from settling in your mouth or throat, spacers help reduce the risk of irritation and minimize the chances of developing oral thrush.
Improved Asthma Control: When you use a spacer, you’re more likely to get the right dose of medication, which can lead to better overall asthma management and fewer flare-ups.
Incorporating a spacer into your routine is a simple way to enhance your inhaler’s effectiveness, improving both your treatment outcomes and comfort